Dangerous Opiate Abuse Side Effects
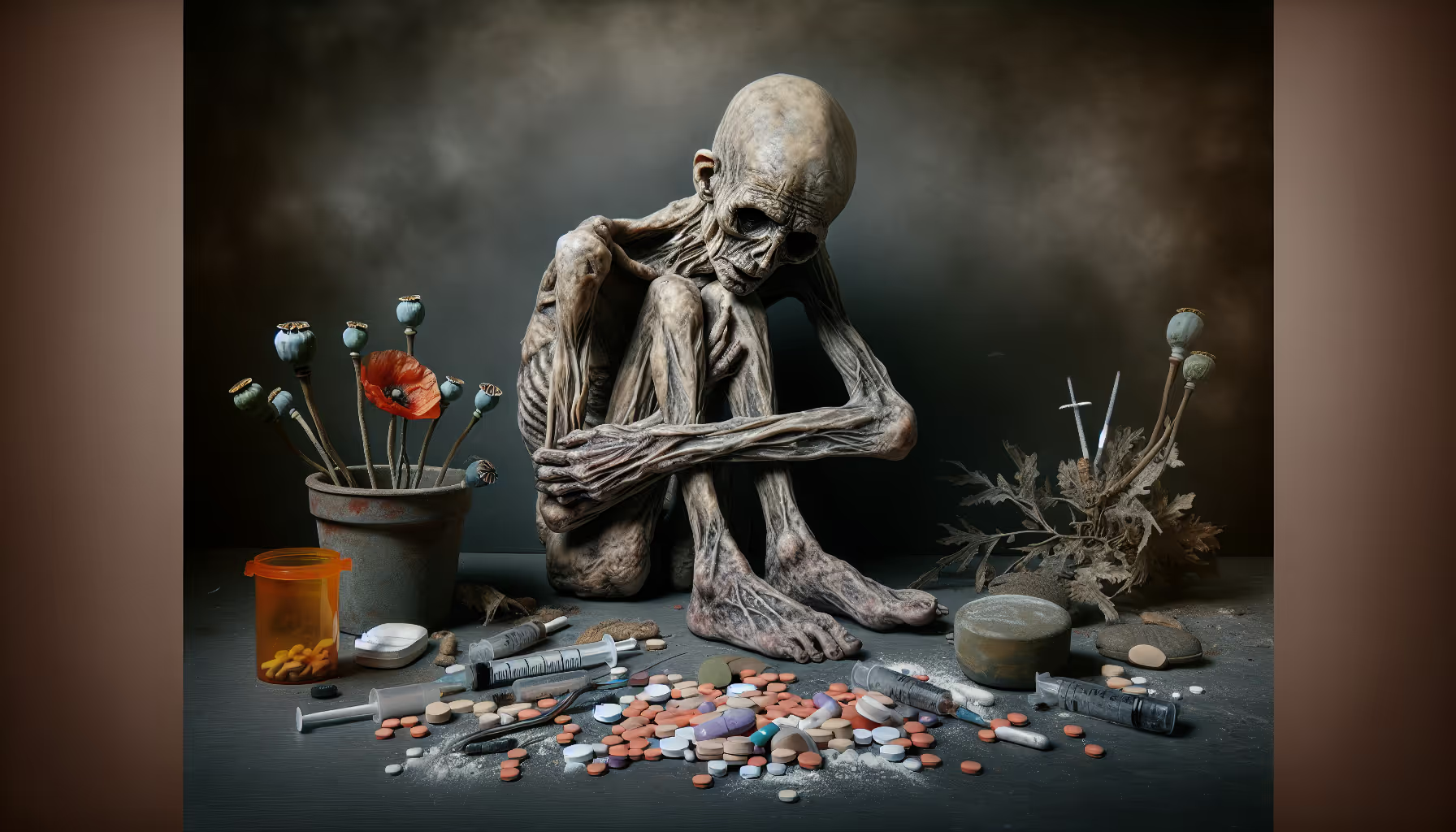
Understanding Opioid Use Disorder
As part of our exploration into the dangerous opiate abuse side effects, it's crucial to first comprehend what Opioid Use Disorder (OUD) is.

Definition and Symptoms
Opioid Use Disorder (OUD) is characterized by a range of symptoms that manifest due to the misuse of opioids, whether they are prescribed medications or illegally obtained substances. Symptoms of this disorder include physical dependence, increasingly heavy, frequent, unhealthy, or risky use, and an overwhelming physical and emotional craving to take the drug.
Opioid addiction, a facet of OUD, shares traits with other chronic relapsing conditions, with signs and symptoms that can be severe. Treatment adherence often presents a challenge. Stressful events, loss of economic stability, and relationship issues can all contribute to an increased risk of relapse in patients with OUD [2].
Risk Factors and Prevalence
Opioid Use Disorder (OUD) is a significant global problem, affecting over 16 million people worldwide and over 2.1 million in the United States. Recreational use of opioids peaked in 2010 and has since decreased as the opioid epidemic gained attention in the United States.
The prevalence of opioid use and dependency varies by age and gender. Men are more likely to use and become dependent on opioids, and opioid-related deaths are highest among individuals between the ages of 40 and 50 years. Heroin overdoses, in contrast, are most common among individuals between the ages of 20 and 30 years.
Understanding Opioid Use Disorder and its prevalence is a critical step in our examination of the side effects of dangerous opiate abuse. The following sections will delve deeper into the effects of opioid abuse, withdrawal symptoms, treatment options, and the impact of opioid overdose.
Effects of Opioid Abuse
Understanding the potential side effects of dangerous opiate abuse is crucial to identify the problem and seek timely intervention. The effects of opioid abuse are seen on both physical and emotional levels, manifesting as cravings and dependence.
Physical and Emotional Cravings
Opioid use disorder (OUD) is characterized by overwhelming physical and emotional cravings to take the drug, among other symptoms. These cravings are the body's response to the absence of the drug, and they can be extremely powerful and difficult to resist.
Withdrawal from opioids can cause symptoms like cravings, sweating, and other physical and emotional urges to take the drug. These symptoms can increase in severity over 72 hours before beginning to ease [1].
The timeline for the onset of withdrawal varies based on the type of opioid used. For instance, heroin withdrawal can begin in as little as five hours, while methadone withdrawal may occur 2 to 3 days following the last ingestion.
Signs of Opioid Dependence
Opioid dependence is another significant effect of opioid abuse. This can manifest as physical dependence, where the body becomes accustomed to the presence of the drug and experiences withdrawal symptoms when the drug is not taken.
Physical dependence on opioids can occur even without unhealthy use, such as in the case of a patient with cancer experiencing chronic pain. However, when combined with increasingly heavy, frequent, unhealthy, or risky use, physical dependence becomes a significant concern.
Opioid withdrawal is a significant complication of OUD, and symptoms may persist for days to weeks, posing a risk of overdose, especially during the transition from detoxification to maintenance therapy [2].
Recognizing these signs and seeking appropriate treatment is crucial in managing opioid dependence and mitigating the dangerous side effects of opiate abuse.
Opioid Withdrawal Symptoms
One of the most challenging aspects of overcoming opioid use disorder (OUD) is managing withdrawal symptoms. These symptoms can be both physical and psychological, manifesting as intense cravings for the drug and a range of other uncomfortable effects. Understanding these symptoms can provide insight into the severity of the problem and the need for effective treatment strategies.
Cravings and Physical Urges
Withdrawal from opioids can cause profound cravings for the drug, which can be both physical and emotional. These cravings are not merely a desire for the drug; they can be overwhelmingly intense, often described as a physical hunger or a deep-seated emotional need. In addition to cravings, people in withdrawal may experience sweating, body aches, and other physical discomforts. These symptoms can peak in severity over a 72-hour period before beginning to ease Johns Hopkins Medicine.
Withdrawal Timeline and Severity
The timeline and severity of opioid withdrawal can vary significantly based on the type of opioid used and the individual's level of dependency. The onset of withdrawal symptoms can range from just a few hours to several days after the last ingestion of the drug. For example, withdrawal symptoms from heroin can begin in as little as five hours, while withdrawal from methadone may not occur until 2 to 3 days following the last ingestion NCBI Bookshelf.
Symptoms can last from a few days to several weeks, depending on the severity of the dependency and the individual's overall health. It's important to note that opioid withdrawal poses a significant risk of overdose, particularly during the transition from detoxification to maintenance therapy.
The side effects of dangerous opiate abuse are not just limited to physical withdrawal symptoms but also extend to significant endocrine and sleep disturbances, especially in women. These challenges highlight the importance of seeking professional help for managing opioid withdrawal.
Treatment Options for Opioid Use Disorder
Addressing the issue of dangerous opiate abuse side effects necessitates an exploration of the available treatment options for opioid use disorder (OUD). These treatment options may include medications specifically designed for OUD and various support programs and therapies aimed at aiding recovery.
Medications for OUD
The use of medications in the treatment of OUD is an important aspect of many successful recovery programs. These medications can help manage withdrawal symptoms, reduce cravings, and bring about a sense of normalcy in brain chemistry, thereby improving the chances of recovery.
According to Johns Hopkins Medicine, medications such as methadone, buprenorphine, or naltrexone may be used as part of the treatment plan.
Moreover, the Mainstreaming Addiction Treatment (MAT) Act has empowered all healthcare providers with a controlled substance certificate to prescribe buprenorphine for OUD, eliminating the previous X-Waiver limitations. This Act aims to destigmatize the standard of care for OUD and integrate substance use disorder treatment across healthcare settings [2].
Here's a brief overview of these medications:
- Methadone: This medication helps reduce withdrawal symptoms and cravings by acting on the same targets in the brain as other opioids, but without the euphoric effect.
- Buprenorphine: This medication, which can be prescribed by certified healthcare providers, reduces withdrawal symptoms and cravings.
- Naltrexone: This medication blocks the effects of opioids, reducing the sense of euphoria or high associated with their use.
Support Programs and Therapies
In addition to medication, various support programs and therapies can be crucial in the treatment of OUD. These programs often include counseling and behavioral therapies that help individuals understand their addiction, develop coping strategies, and work towards a life free of opioid dependence.
According to the American Psychiatric Association, only about one in four people with opioid use disorder receive specialty treatment. However, such treatments, including medications for opioid use disorder (MOUD), counseling, and behavioral therapies, have been shown to help people stay in treatment, reduce opioid use, overdoses, and risks associated with opioid use disorder.
Support programs and therapies can take many forms, including:
- Individual or Group Counselling: This form of therapy involves regular sessions with a counselor or therapist, either one-on-one or in a group setting.
- Cognitive Behavioral Therapy (CBT): This form of therapy helps individuals recognize and change patterns of negative thinking and behavior.
- Motivational Interviewing: This is a counseling method that helps individuals resolve ambivalent feelings to find the internal motivation they need to change their behavior.
- 12-Step Facilitation Therapy: This is a structured approach to recovery that involves acceptance, surrender, and active involvement in 12-step recovery programs.
By combining medication with support programs and therapies, individuals suffering from OUD can navigate the road to recovery more effectively and manage the side effects of dangerous opiate abuse. The use of these treatments underscores the importance of a comprehensive approach in addressing the broad impacts of opioid use disorder.
Impact of Opioid Overdose
Opioid overdose is a life-threatening condition resulting from the abuse of opiates, with over 16 million people worldwide and over 2.1 million in the United States affected by Opioid Use Disorder (OUD). This section discusses the risk factors for opioid overdose and the role of naloxone in its prevention and treatment.
Risk Factors and Prevention
Opioid overdose may occur as a result of OUD, with a high risk in untreated patients as well as in patients who have received treatment. The period between detoxification and the start of maintenance therapy poses the highest risk for treated patients. Cognitive behavioral therapy may help decrease this risk [2].
Synthetic opioids, especially fentanyl which is 50 times more potent than heroin and 100 times more potent than morphine, pose a significant threat. By June 2021, they were involved in an estimated 87% of opioid deaths and 65% of all drug overdose deaths [3].
Prevention strategies should focus on the early identification of OUD and the initiation of appropriate treatment. Efforts should also be geared towards reducing the availability and misuse of synthetic opioids.
Naloxone Administration
Naloxone is an antidote to opioids that can reverse the effects of an opioid overdose if administered in time. It has virtually no effect on individuals who have not taken opioids.
Recent programs worldwide have demonstrated that providing naloxone to people likely to witness an opioid overdose, coupled with training on naloxone use and resuscitation following an overdose, can significantly reduce opioid overdose deaths. This is particularly relevant for people with OUD and those leaving prison, as they have very high rates of opioid overdose during the first four weeks after release.
In the event of an opioid overdose, the timely administration of naloxone can effectively prevent death. As part of the broader strategy to combat the dangerous side effects of opiate abuse, it is essential to increase awareness and access to this life-saving medication.
Women and Opioid Use
The dangerous side effects of opiate abuse can be particularly severe for women due to their unique biological and psychosocial factors. These include a range of risks from endocrinopathy and reduced fertility to neonatal risks and the risk of unintentional overdose.
Unique Risks for Women
According to NCBI, women face unique risks due to long-term opioid use, including reduced fertility, greater risk for polypharmacy, cardiac risks, poisoning, and unintentional overdose among other risks. Women are more likely than men to have a chronic pain condition, to be treated with opioids, and may receive higher doses. Across age groups, long-term opioid use was greater in women compared with men, and highest among older women. Older women taking ≥50 mg/day of morphine equivalents have a twofold increased risk of fracture.
Impact on Pregnancy and Sleep
The impacts of opioids on women extend to pregnancy and sleep as well. Chronic opioid use during pregnancy has been associated with low birth weight, premature birth, hypoxic-ischemic brain injury, prolonged QT syndrome, neonatal withdrawal syndrome, and neonatal death. Maternal exposure to opioids was associated with cardiac defects in neonates and noncardiac birth defects.
These findings emphasize the importance of understanding the gender-specific effects of opioid use and developing targeted interventions to prevent and treat opioid use disorder in women.
References
[1]: https://www.hopkinsmedicine.org/health/conditions-and-diseases/opioid-use-disorder
[2]: https://www.ncbi.nlm.nih.gov/books/NBK553166/
[3]: https://www.psychiatry.org/patients-families/opioid-use-disorder
[4]: https://www.who.int/news-room/fact-sheets/detail/opioid-overdose
[5]: https://my.clevelandclinic.org/health/drugs/21127-opioids
You’re not alone in this.
When mental health challenges and addiction intersect, it can feel isolating. At Arista, we offer compassionate, evidence-based, and trauma-informed care to help you heal, grow, and move forward.
You’re not alone in this.
When mental health challenges and addiction intersect, it can feel isolating. At Arista, we offer compassionate, evidence-based, and trauma-informed care to help you heal, grow, and move forward.
Support that moves with you.
You’ve taken a brave first step. At Arista Recovery, we’re here to help you continue with best-in-class care designed for long-term healing and support.
.webp)






